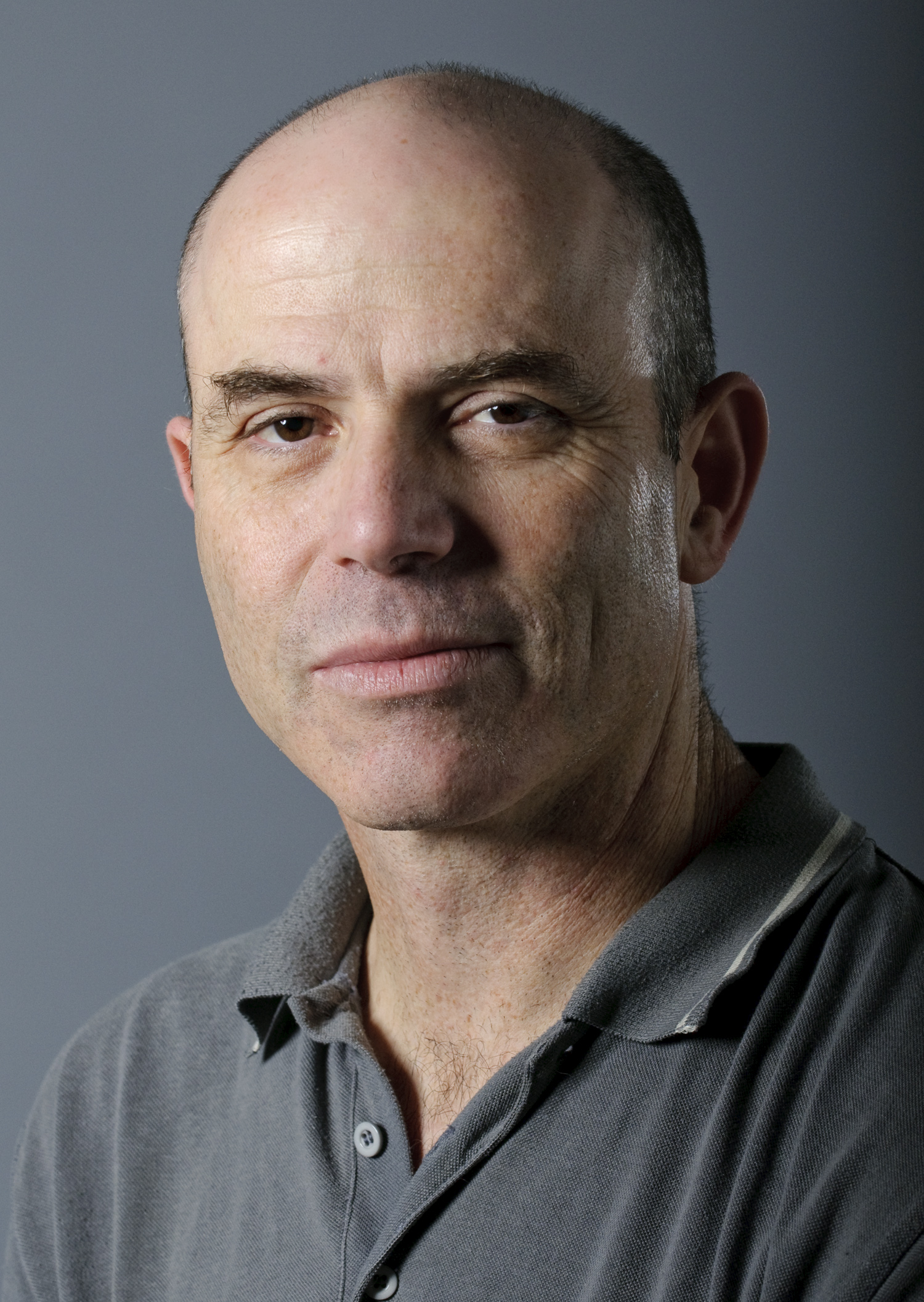
Research Field
Dr. Rudich studies obesity and related diseases (e.g., cardiometabolic disorders, such as type 2 diabetes), focusing on how changes in adipose tissue (i.e., fat) biology contribute to these diseases from a metabolic perspective. In addition, obesity may be the number one or two preventable cause of certain cancers, such as colon, pancreatic, liver, endometrial, and gastro-intestinal – there is a 1.5-to-3-fold increase of incidence in these cancers if someone is obese. Incidentally, these are also the most lethal cancers. Meanwhile, non-alcoholic fatty liver disease (NAFLD) presents in one-third of the adult population in Western societies – en route to liver cancer – with no specific ways to treat it, and 50-70% of obese people have NAFLD.
The research group looks at the potential contribution of adipose tissues to this – which types of adipose tissue contribute to these different diseases and by which mechanisms? Which types are more protective? For example, the researchers have observed that sometimes a metabolically normal obese person is spared from some of the classical metabolic consequences of their obesity.
To do this the research team concentrates on two major axes: the first is the interaction of adipose with immune cells at the interface between metabolism and immunity (i.e., immunometabolism), since immune cells must alter metabolism to become active. The second axis is an endocrine axis of adipose tissue within the abdominal cavity (i.e., visceral fat) and the liver – the abdominal cavity, including the visceral fat, is drained by the portal vein into the liver, so anything that is secreted by this fat depot goes directly into the liver.
The Rudich lab is developing an animal model for the reversal of obesity. The vast majority of research in this field relates to obesity and its related pathologies or illnesses. The real world situation, though, is that obese people want to be lean, but very little is known about the processes involved and how it promotes metabolic health. So researchers try to look at it from an adipocentric perspective – do the changes need to be reversed in the adipose tissue for recovery?
The research group has found that when we feed mice a high fat diet and then reverse it to a normal diet, we see reversal of the dysmetabolic stage, e.g., recovery of glucose levels and insulin resistance, much sooner than a reversal of the obesity is observed. So while many of the processes in adipose tissue are still there and the obesity itself has yet to be resolved, from a metabolic perspective recovery has occurred, especially in the liver.
Prof. Rudich’s group has identified some microRNAs (miRNAs, small, non-coding, regulatory molecules) whose expression levels change between lean, obese, and ‘reversed’ individuals, so they are using antagomirs to target these in the hope to gain a metabolic advantage in obese animals. The aim is to create a microRNA-based drug that imitates obesity reversal in terms of the metabolic outcome, making it less unhealthy for those who suffer from the consequences of obesity (for some people obesity takes less of a toll on the body, at least in terms of the cardiometabolic effects). To that end, the researchers have developed the capacity to deliver molecules (antagomirs) to mice that target microRNA via a tail vein injection and demonstrated that these can reverse the effects of these microRNA on their targets. The dream is to establish microRNA-based therapy for relieving the effects of obesity on the liver and on whole-body metabolism, mimicking obesity reversal.
 ?>)